I’ve been putting this off.
But recent events reminded me it’s best not to delay. So, let’s talk about cancer.
TLDR
Cancer is complex. I launched into the subject with screening and prevention at the front of my mind and quickly learned some simple truths and underlying complexities.
Screening for everything isn’t feasible today: Early detection saves lives, but screening isn’t a one-size-fits-all solution. It has costs (time, money, physical risks, psychological stress) and benefits that depend on individual factors like age, family history, and risk level.
What’s cancer, really? It’s not one disease but a category of diseases involving uncontrolled cell growth. Early detection dramatically improves survival rates—Stage 1 cancers often have over 90% five-year survival rates, compared to much lower rates at Stage 4.
My approach: Is to make cancer detection a partnership between me in my doctor, in which I play an active role. I’ve learned to pay attention to my body, understand warning signs, explore my family history, and proactively raise the topic with my doctor.
My screening journey so far: focusing on the most common cancers for women and where I’m at higher risk:
Breast cancer: Booked my first mammogram at 43, self-funded, after learning that starting at 40 is wise
Bowel cancer: Had a colonoscopy at 39 due to being high risk. If not for that, I personally would self-fund one today
Cervical cancer: A no-brainer in my view. HPV testing now makes screening easier and potentially less frequent
Melanoma: Regular skin checks and mole mapping help me manage my higher risk from fair skin and environmental exposure.
This is my the beginning—and there’s more to learn as science advances. Wherever you are today, take one step forward. Early detection could make all the difference.
Let’s screen for everything!
As a person focussed on prevention and healthspan, the first thing I was drawn to explore was cancer screening.
I knew that survival rates are dramatically better when cancer was caught early. It gave me the urge to get screened for every cancer under the sun.
But it’s not that simple.
Cancer screening comes with both benefits and costs.
The costs can include:
Time and money - which can be significant and may need to be met out-of-pocket
Physical risks - such as radiation, infection, injury
False positives and false negatives - tests aren’t perfect, some less than others
Overdiagnosis and overtreatment - arising from misdiagnosis or treating cancers that would not have caused harm
Physhological stress - associated with screening, awaiting results, diagnosis whether accurate or not and potential treatment
The benefits also vary depending on factors like the effectiveness of the test, your age, family history and environment, and the availability of effective treatments.
Take lung cancer, for example. It’s relatively common, but we don’t screen everyone. Heavy smokers clearly benefit. But much lower prevalence in non-smokers mean the costs usually outweigh the benefits — testing is expensive, involves radiation exposure and often leads to false positives, overdiagnosis and overtreatment.
In short, I’d need cancer screening tailored to me as an individual. And what’s right for me might not be be right for you.
But before trying to figure out more about screening, I had a more fundamental question:
What is cancer, really?
Cancer is the second leading cause of death worldwide and affects roughly half of all people who live to 80.
We all know someone directly affected with cancer or we’re dealing with it ourselves.
Despite its prevalence, my understanding of cancer was a patchwork of information picked up from conversations and media portrayals.
Here are some basics that I’ve learned.
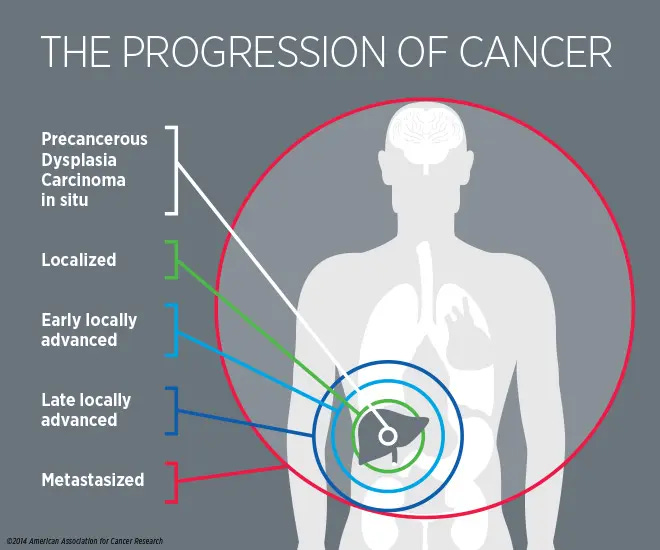
Cancer isn’t one disease—it’s a category. It happens when abnormal cells grow uncontrollably, disrupting the normal cycle where damaged cells die and new ones take their place. These rogue cells can accumulate to form tumors or crowd out healthy cells in blood or bone marrow.
Cancer progresses over time if untreated. You’ve probably heard of the stages (1-4):
• Stage 1: Small and localized.
• Stage 4: Larger and spread to distant areas (metastasis).
As cancer advances, treatments become more complex and survival rates drop.
How much early detection matters
Survival rates vary massively depending on how early cancer is detected.
I didn’t realise how much.
The charts below show relative five year survival rates for breast cancer and colorectal (bowel) cancer for women.
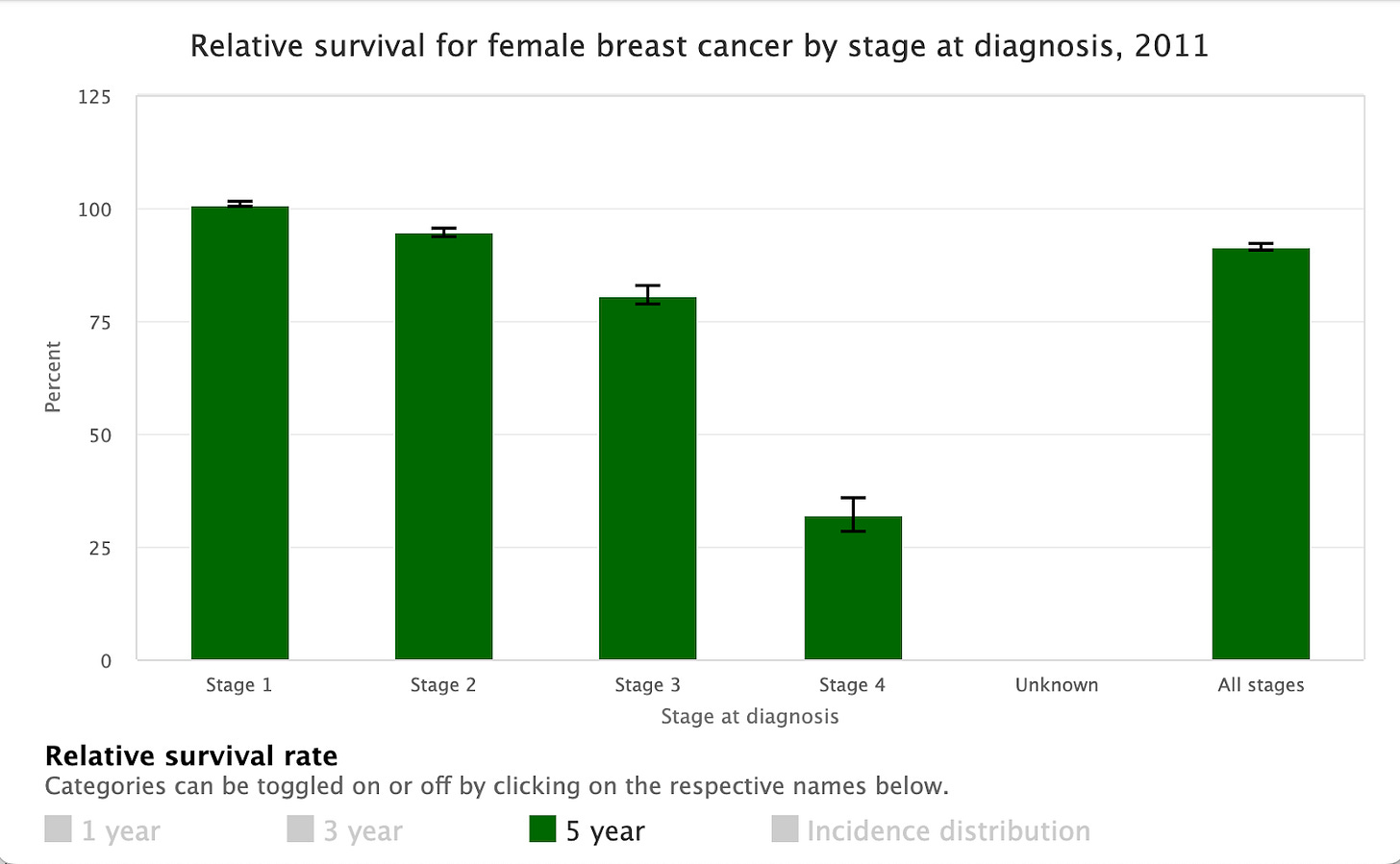

For these cancers, five year survival when detected at Stage 1 is well above 90% (even higher in this data, which is from Australian women).1
I was also struck by the survival rates for Stages 2 and 3 — they were higher than I might have guessed.
In stark contrast, five year survival rates when diagnosed at Stage 4 are much, much lower.
No one wants to find out they have cancer. But seeing this data hammered the message home for me - I’d rather find out sooner than later.
Prevention, detection and screening
A healthy lifestyle is the first order of business for cancer prevention. But even the healthiest lifestyle can’t eliminate all cancer risk.
So how do I manage my risk? And since ‘screening for everything’ isn’t advisable, how can I understand what screening is right for me?
Here’s where I’ve landed:
Partnership - I need to work in partnership with my doctor. Personal responsibility combined with expert guidance is the most powerful combination. No one should try to manage cancer risk on their own, it’s way too complex.
Proactivity - It’s commonplace that cancer risk isn’t discussed with doctors until symptoms arise. Like all doctors, mine is busy and might not proactively raise cancer while I present as healthy. But I can be the one to start the conversation.
Preparation - For well informed conversations about risk by bringing my share of the information, through:
Paying attention to my body — I have to first know what’s normal for me if I am to spot something unusual
Learn the warning signs — especially for common cancers, like breast cancer, or where I’m at higher risk, like skin cancer.
Understand my family history — I was missing important details regarding the experience of family members. It’s a delicate subject, but one conversation with my mum gave me much greater clarity on our family’s cancer history—and ensured my kids won’t have to start from scratch someday.
Consider environmental risks — Honest discussions about lifestyle and exposures are crucial.
Curiosity about screening — I learned a bit about screening options I thought might be relevant so that I could discuss them. More about this in the next section.
Starting a conversation with a doctor can feel intimidating, but I’ve learned that most doctors are open and receptive. Here’s how I initiated it:
I’m keen to be proactive about managing my cancer risk. What should I focus on for my age, family history and circumstances?
Are there any screening tests we should go ahead with now or soon?
I’d like to hear about options even if I’d need to pay for them myself.
Finally, I’ve made a commitment to myself that if something looks or feels off, I won’t delay speaking to a doctor or nurse. It’s so easy to let seemingly minor things slide.
Screening & me
There are all sorts of exciting emerging technologies when it comes to screening, which I’m curious to learn about in future - liquid biopsies, genetic testing, AI.
But first, I’ve started with the basics. My screening journey so far focusses on:
The most common cancers for women
Cancers linked to my genetics or family history
Risks unique to my environment
I’m sharing this as a one woman example. Remember, what’s right for me might not be the same for you.
Quick note: 👉 Please feel free to share this post with friends or to click the ❤️ button so more people can discover it on Substack 🙏
Breast Cancer & me
Breast cancer is the most common cancer for women globally. Regular mammograms unquestionably save lives.
Evidence now suggests women of average risk should start mammograms at age 40. Indeed, breast cancer tends to develop more aggressively among women in their 40s than in older women.2
In New Zealand where I live, free mammograms start at 45, but you can get them from 40 if you’re prepared to pay.3
I cleared up a couple more of my misconceptions:
My doctor hasn’t suggested I start mammograms, so it means I don’t need to. Wrong - when I asked my doctor, she agreed starting at 40 is wise
I’m breastfeeding, so it’s not a good time for a mammogram. Also wrong - breastfeeding women can have a mammogram.
Knowing what I now do and as fortunately I can afford the cost, I’ve booked for my first mammogram next month rather than waiting until I’m eligible for free.
Bowel (colorectal) Cancer & me
Bowel cancer is the third most common cancer for women.4
Again, there’s a gap between when screening would ideally begin based on evidence and what’s currently being funded.
Expert organisations such as the American Cancer Society and the US Preventative Services Taskforce recommend screening from age 45. Longevity specialist Dr Peter Attia encourages screening from age 40. The publicly funded screening programme in New Zealand begins at age 60.5
Colonoscopy is the gold standard for screening because they are highly effective at detecting cancer and also enable the identification and removal of precancerous polyps. But there are downsides. It’s expensive (around $2,500), invasive and has some physical risks and discomforts - bowel preparation; potential for bleeding and in the rare case perforation; sedation or my personal favourite having meters of hose stuck up your bum without sedation.
I had a colonoscopy at age 39. A beloved close relative is living with bowel cancer and this put me in a high risk category.
If this hadn’t been the case, would I self-fund a colonoscopy now?
Yes, absolutely, I would.
It’s expensive and a bit unpleasant, but usually only required once every 10 years. And bowel cancer is perhaps the most preventable of all cancer mortality, due to the effectiveness of colonoscopy.
Would I once again do it without sedation? Ha ha … that’s a harder sell. Ask me in a year when I’m due for another one!
Cervical Cancer & me
Cervical cancer is the fourth most common cancer for women worldwide.
My assessment is that cervical cancer screening is a no-brainer — simple, low cost and effective a detecting abnormal cells even before cancer begins. The hardest part used to be keeping up to date with appointments every three years.
Recently, I was delighted to find that screening has become even easier with the introduction of HPV testing in New Zealand and other countries. It’s minimally invasive (you can collect the sample yourself) and only required every five years if abnormalities or high risks are not present.
Screening should start at 25 and continue until 65.
Screening often does detect HPV (human papillomavirus, a sexually transmitted infection), as it’s extremely common within the population.
Don’t be alarmed. HPV is the root cause of almost all cervical cancers and can cause other cancers too. But HPV does not mean you have or will develop cancer. It means some further testing and monitoring is recommended. Most cases of HPV clear up on their own without causing any health problems.
Even better than screening is prevention through the HPV vaccination which is provided free to women and girls 9-25 years old.6
Melanoma
Thanks to my fair skin and ozone-hole childhood, I’m at higher risk. Annual skin checks and mole mapping help me stay on top of things.
My genetics and environmental exposures put me at higher risk here.
While not in the top 5 globally, melanoma is a leading cause of cancer mortality for women where I live — New Zealand has among the world’s highest rates of skin cancer.
I’m fair-skinned and grew up at the beach under peak ozone hole. Unsurprisingly, many of my relatives have experienced skin cancer (though not melanoma, to my knowledge).
I have annual skin checks with a dermatologist to stay on top of things. I also get a mole map every few years as I like the records it creates. I’ve also become more vigilant at getting unknown spots checked if I find one — in fact, I had one seen this week. The peace of mind is so worth it.
Solid beginning
From a naïve starting point, I gained a more solid footing for managing my cancer risks and screening. It will be an ongoing journey — I will continue to change and technology will too. But for now, I’ve got my next steps lined up against a plan that makes sense for me.
Wherever you are today, I hope this inspires you to take a step forward too.
🙏 If you get value from Extend, please subscribe or click the ❤️ button so that more people can find it on Substack. I’m also grateful when people comment or share posts.
You may notice that for Stage 1 the bar or the error bar (confidence interval shown in black) actually exceeds 100 %. Survival over 100% means that survival among the people diagnosed with cancers exceeded survival in the general population of equivalent age and sex.
The American Cancer Society, United States Preventative Services Task Force and the Breast Cancer Foundation NZ all recommend that screening commence at age 40. The ACS recommends annual screening in women aged 40-55 as breast cancers in this group can be more aggressive.
Screening is not currently recommended for women below 40 who are of average risk, as breast cancer is less common and accurate screening is more difficult.
Lung cancer is second, with the distribution of risk heavily weighted towards smokers and former smokers.
50 for Maori and Pasifika.
HPV vaccination wasn’t around when I was under 25. Is it worth being vaccinated if you’re older? If you’re under 45 then it possibly is, especially on the younger end. Ask your doctor about it if you’re wondering. I understand it costs about $900. At age 43 and given my personal circumstances, I’m not pursuing it for myself but will certainly encourage my daughter.






Thanks Rebecca, I appreciate that. You’re right … all of my skin checks are covered under my insurance and I think that provides me with a lot of value
Great article this month. It’s a good reminder to check all the benefits of your health insurance (if you’re privileged enough to have it) and fully use them.